TLR4
| TLR4 | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | |||||||||||||||||||||||||
| |||||||||||||||||||||||||
| Identifiers | |||||||||||||||||||||||||
| Aliases | TLR4, ARMD10, CD284, TLR-4, TOLL, toll like receptor 4 | ||||||||||||||||||||||||
| External IDs | OMIM: 603030 MGI: 96824 HomoloGene: 41317 GeneCards: TLR4 | ||||||||||||||||||||||||
| |||||||||||||||||||||||||
| |||||||||||||||||||||||||
| |||||||||||||||||||||||||
| |||||||||||||||||||||||||
| Orthologs | |||||||||||||||||||||||||
| Species | Human | Mouse | |||||||||||||||||||||||
| Entrez |
|
| |||||||||||||||||||||||
| Ensembl |
|
| |||||||||||||||||||||||
| UniProt |
|
| |||||||||||||||||||||||
| RefSeq (mRNA) |
|
| |||||||||||||||||||||||
| RefSeq (protein) |
|
| |||||||||||||||||||||||
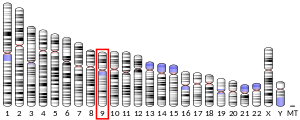
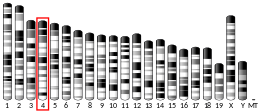
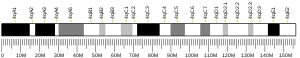
| Location (UCSC) | Chr 9: 117.7 – 117.72 Mb | Chr 4: 66.83 – 66.93 Mb | |||||||||||||||||||||||
PubMed search | [3] | [4] | |||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||
| |||||||||||||||||||||||||
Toll-like receptor 4 is a protein that in humans is encoded by the TLR4 gene. TLR4 is a transmembrane protein, member of the toll-like receptor family, which belongs to the pattern recognition receptor (PRR) family. Its activation leads to an intracellular signaling pathway NF-κB and inflammatory cytokine production which is responsible for activating the innate immune system.[5] It is most well-known for recognizing lipopolysaccharide (LPS), a component present in many Gram-negative bacteria (e.g. Neisseria spp.) and select Gram-positive bacteria. Its ligands also include several viral proteins, polysaccharide, and a variety of endogenous proteins such as low-density lipoprotein, beta-defensins, and heat shock protein.[6]
TLR4 has also been designated as CD284 (cluster of differentiation 284). The molecular weight of TLR4 is approximately 95 kDa.
Contents
1 Function
2 Signaling
2.1 MyD88 – Dependent Pathway
2.2 MyD88 – Independent Pathway
2.3 SARM: Negative Regulator of the TRIF-mediated Pathway
3 Evolutionary history
4 Interactions
5 Clinical significance
5.1 In insulin resistance
5.2 In cancer progression
5.3 In pregnancy
5.4 Asp299Gly polymorphism
6 Animal studies
7 Drugs targeting TLR4
7.1 Agonists
7.2 Antagonists
8 References
9 External links
Function
The protein encoded by this gene is a member of the toll-like receptor (TLR) family, which plays a fundamental role in pathogen recognition and activation of innate immunity. TLRs are highly conserved from Drosophila to humans and share structural and functional similarities. They recognize pathogen-associated molecular patterns (PAMPs) that are expressed on infectious agents, and mediate the production of cytokines necessary for the development of effective immunity.
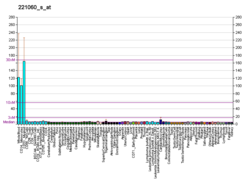
The various TLRs exhibit different patterns of expression. This receptor is most abundantly expressed in placenta, and in myelomonocytic subpopulation of the leukocytes.
It cooperates with LY96 (also referred as MD-2) and CD14 to mediate in signal transduction events induced by lipopolysaccharide (LPS)[7] found in most gram-negative bacteria. Mutations in this gene have been associated with differences in LPS responsiveness.
TLR4 signaling responds to signals by forming a complex using an extracellular leucine-rich repeat domain (LRR) and an intracellular toll/interleukin-1 receptor (TIR) domain. LPS stimulation induces a series of interactions with several accessory proteins which form the TLR4 complex on the cell surface. LPS recognition is initiated by an LPS binding to an LBP protein. This LPS-LBP complex transfers the LPS to CD14. CD14 is a glycosylphosphatidylinositol-anchored membrane protein that binds the LPS-LBP complex and facilitates the transfer of LPS to MD-2 protein, which is associated with the extracellular domain of TLR4. LPS binding promotes the dimerization of TLR4/MD-2. The conformational changes of the TLR4 induce the recruitment of intracellular adaptor proteins containing the TIR domain which is necessary to activate the downstream signaling pathway.[8]
Several transcript variants of this gene have been found, but the protein-coding potential of most of them is uncertain.[9]
Most of the reported effects of TLR4 signaling in tumors are pro-carcinogenic mainly due to contributions of proinflammatory cytokine signaling (whose expression is driven by TLR-mediated signals) to tumor-promoting microenvironment.[10]
Signaling
Upon LPS recognition, conformational changes in the TLR4 receptors result in recruitment of intracellular TIR-domains containing adaptor molecules. These adaptors are associated with the TLR4 cluster via homophilic interactions between the TIR domains. There are four adaptor proteins involved in two major intracellular signaling pathways.[11]

Signaling pathway of toll-like receptor 4. Dashed grey lines represent unknown associations
MyD88 – Dependent Pathway
The MyD88-dependent pathway is regulated by two adaptor-associated proteins: Myeloid Differentiation Primary Response Gene 88 (MyD88) and TIR Domain-Containing Adaptor Protein (TIRAP). TIRAP-MyD88 regulates early NF-κβ activation and production of proinflammatory cytokines, such as IL-12.[5] MyD88 signaling involves the activation of IL-1 Receptor-Associated Kinases (IRAKs) and the adaptor molecules TNF Receptor-Associated Factor 6 (TRAF6). TRAF6 induces the activation of TAK1 (Transforming growth factor-β-Activated Kinase 1) that leads to the activation of MAPK cascades (Mitogen-Activated Protein Kinase) and IKK (IκB Kinase). IKKs' signaling pathway leads to the induction of the transcription factor NF-κB, while activation of MAPK cascades lead to the activation of another transcription factor AP-1. Both of them have a role in the expression of proinflammatory cytokines.[8] The activation of NF-κB via TAK-1 is complex, and it starts by the assembly of a protein complex called the signalosome, which is made of a scaffolding protein, called NEMO. The protein complex is made from two different κB kinases, called IKKα and IKKβ. This causes the addition of a small regulatory protein to the signalosome called ubiquitin, that acts to initiate the release of the NF-κB protein, which coordinates translocation in the nucleus of cytokines.[12]
MyD88 – Independent Pathway
This TRIF-dependent pathway involves the recruitment of the adaptor proteins TIR-domain-containing adaptor inducing interferon-β (TRIF) and TRIF-related Adaptor Molecule (TRAM). TRAM-TRIF signals activate the transcription factor Interferon Regulatory Factor-3 (IRF3) via TRAF3. IRF3 activation induces the production of type 1 interferons.[11]
SARM: Negative Regulator of the TRIF-mediated Pathway
A fifth TIR-domain-containing adaptor protein called Sterile α and HEAT (Armadillo motif) (SARM) is a TLR4 signaling pathway inhibitor. SARM activation by LPS-binding inhibits -TRIF-mediated pathways but does not inhibit MyD88-mediated pathways. This mechanism prevents an excessive activation in response to LPS which may lead to inflammation-induced damage such as sepsis.[8]
Evolutionary history
TLR4 originated when TLR2 and TLR4 diverged about 500 million years ago near the beginning of vertebrate evolution.[13] Sequence alignments of human and great ape TLR4 exons have demonstrated that not much evolution has occurred in human TLR4 since our divergence from our last common ancestor with chimpanzees; human and chimp TLR4 exons only differ by three substitutions while humans and baboons are 93.5% similar in the extracellular domain.[14] Notably, humans possess a greater number of early stop codons in TLR4 than great apes; in a study of 158 humans worldwide, 0.6% had a nonsense mutation.[15][16] This suggests that there are weaker evolutionary pressures on the human TLR4 than on our primate relatives. The distribution of human TLR4 polymorphisms matches the out-of-Africa migration, and it is likely that the polymorphisms were generated in Africa before migration to other continents.[16][17]
Interactions
TLR4 has been shown to interact with:
Lymphocyte antigen 96,[18][19]
Myd88,[20][21][22][23] and
TOLLIP.[24]
Nickel, [25]
Intracellular trafficking of TLR4 is dependent on the GTPase Rab-11a, and knock down of Rab-11a results in hampered TLR4 recruitment to E. coli-containing phagosomes and subsequent reduced signal transduction through the MyD88-independent pathway.[26]
Clinical significance
Various single nucleotide polymorphisms (SNPs) of the TLR4 in humans have been identified[27] and for some of them an association with increased susceptibility to Gram-negative bacterial infections [28] or faster progression and a more severe course of sepsis in critically ill patients was reported.[29]
In insulin resistance
Fetuin-A facilitates the binding of lipids to receptors, thereby inducing insulin resistance.[30]
In cancer progression
TLR4 expression can be detected on many tumor cells and cell lines. TLR4 is capable of activating MAPK and NF-κB pathways, implicating possible direct role of cell-autonomous TLR4 signaling in regulation of carcinogenesis, in particular, through increased proliferation of tumor cells, apoptosis inhibition and metastasis. TLR4 signaling may also contribute to resistance to paclitaxel chemotherapy in ovary cancer and siRNA therapy in prostate cancer. 63% of breast cancer patients were reported to express TLR4 on tumor cells and the level of expression inversely correlated with the survival. Additionally, low MyD88 expression correlated with decreased metastasis to the lung and decreased CCL2 and CCL5 expression. TLR4 expression levels were the highest among TLRs in human breast cancer cell line MDA-MB-231 and TLR4 knockdown resulted in decreased proliferation and decreased IL-6 and IL-8 levels. On the other hand, TLR4 signaling in immune and inflammatory cells of tumor microenvironment may lead to production of proinflammatory cytokines (TNF, IL-1β, IL-6, IL-18, etc.), immunosuppressive cytokines (IL-10, TGF-β, etc.) and angiogenic mediators (VEGF, EGF, TGF-β, etc.). These activities may result in further polarization of tumor-associated macrophages, conversion of fibroblasts into tumor-promoting cancer-associated fibroblasts, conversion of dendritic cells into tumor-associated DCs and activation of pro-tumorigenic functions of immature myeloid cells - Myeloid-derived Suppressor Cells (MDSC). TLR signaling has been linked to accumulation and function of MDSC at the site of tumor and it also allows mesenchymal stromal cells to counter NK cell-mediated anti-tumor immunity. In HepG2 hepatoblastoma cells LPS increased TLR4 levels, cell proliferation and resistance to chemotherapy, and these phenomena could be reversed by TLR4 gene knockdown. Similarly, LPS stimulation of human liver cancer cell line H7402 resulted in TLR4 upregulation, NF-κB activation, TNF, IL-6 and IL-8 production and increased proliferation that could be reversed by signal transducer
and STAT3 inhibition.Besides the well known successful usage of Bacillus Calmette–Guérin (BCG) in the therapy of bladder cancer there are reports on the treatment of oral squamous cell carcinoma, gastric cancer and cervical cancer with lyophilized streptococcal preparation OK-432 and utilization of TLR4/TLR2 ligands – derivatives of muramyl dipeptide.[10]
In pregnancy
Activation of TLR4 in intrauterine infections leads to deregulation of prostaglandin synthesis, leading to uterine smooth muscle contraction.
Asp299Gly polymorphism
Classically, TLR4 is said to be the receptor for LPS, however TLR4 has also been shown to be activated by other kinds of lipids. Plasmodium falciparum, a parasite known to cause the most common and serious form of malaria that is seen primarily in Africa, produces glycosylphosphatidylinositol, which can activate TLR4.[31] Two SNPs in TLR4 are co-expressed with high penetrance in African populations (i.e. TLR-4-Asp299Gly and TLR-4-Thr399Ile). These Polymorphisms are associated with an increase in TLR4-Mediated IL-10 production—an immunomodulator—and a decrease in proinflammatory cytokines.[32] The TLR-4-Asp299Gly point mutation is strongly correlated with an increased infection rate with Plasmodium falciparum. It appears that the mutation prevents TLR4 from acting as vigorously against, at least some plasmodial infections. The malaria infection rate and associated morbidity are higher in TLR-4-Asp299Gly group, but mortality appears to be decreased. This may indicate that at least part of the pathogenesis of malaria takes advantage of cytokine production. By reducing the cytokine production via the TLR4 mutation, the infection rate may increase, but the number of deaths due to the infection seem to decrease.[31]
In addition, TLR4-D299G has been associated with aggressive colorectal cancer in humans. It has been shown that human colon adenocarcinomas from patients with TLR4-D299G were more frequently of an advanced stage with metastasis than those with wild-type TLR4. The same study demonstrated functionally that intestinal epithelial cells (Caco-2) expressing TLR4-D299G underwent epithelial-mesenchymal transition and morphologic changes associated with tumor progression, whereas intestinal epithelial cells expressing wild-type TLR4 did not.[33]
Animal studies
A link between the TLR4 receptor and binge drinking has been suggested. When genes responsible for the expression of TLR4 and GABA receptors are manipulated in rodents that had been bred and trained to drink excessively, the animals showed a "profound reduction" in drinking behaviours.[34] Additionally, it has been shown that ethanol, even in the absence of LPS, can activate TLR4 signaling pathways.[35]
High levels of TLR4 molecules and M2 tumor-associated macrophages are associated with increased susceptibility to cancer growth in mice deprived of sleep. Mice genetically modified so that they could not produce TLR4 molecules showed normal cancer growth.[36]
Drugs targeting TLR4
Toll-like receptor 4 has been shown to be important for the long-term side-effects of opioid analgesic drugs. Various μ-opioid receptor ligands have been tested and found to also possess action as agonists or antagonists of TLR4, with opioid agonists such as morphine being TLR4 agonists, while opioid antagonists such as naloxone were found to be TLR4 antagonists. Activation of TLR4 leads to downstream release of inflammatory modulators including TNF-α and Interleukin-1, and constant low-level release of these modulators is thought to reduce the efficacy of opioid drug treatment with time, and be involved in both the development of tolerance to opioid analgesic drugs,[37][38] and in the emergence of side-effects such as hyperalgesia and allodynia that can become a problem following extended use of opioid drugs.[39][40] Drugs that block the action of TNF-α or IL-1β have been shown to increase the analgesic effects of opioids and reduce the development of tolerance and other side-effects,[41][42] and this has also been demonstrated with drugs that block TLR4 itself. The response of TLR4 to opioid drugs has been found to be enantiomer-independent, so the "unnatural" enantiomers of opioid drugs such as morphine and naloxone, which lack affinity for opioid receptors, still produce the same activity at TLR4 as their "normal" enantiomers.[43][44] This means that the unnatural enantiomers of opioid antagonists, such as (+)-naloxone, can be used to block the TLR4 activity of opioid analgesic drugs, while leaving the μ-opioid receptor mediated analgesic activity unaffected.[45])[44][46] This may also be the mechanism behind the beneficial effect of ultra-low dose naltrexone on opioid analgesia.[47]
Morphine causes inflammation by binding to the protein lymphocyte antigen 96, which, in turn, causes the protein to bind to Toll-like receptor 4 (TLR4).[48] The morphine-induced TLR4 activation attenuates pain suppression by opioids and enhances the development of opioid tolerance and addiction, drug abuse, and other negative side effects such as respiratory depression and hyperalgesia. Drug candidates that target TLR4 may improve opioid-based pain management therapies.[49]
Agonists
Buprenorphine[50]
Carbamazepine[51]
Ethanol[52]
Fentanyl[50]
Levorphanol[50]
Lipopolysaccharides (LPS)[53]
Methadone[50]
Morphine[50]
Oxcarbazepine[51]
Oxycodone[50]
Pethidine[50]
- Glucuronoxylomannan from Cryptococcus[54][55]
Morphine-3-glucuronide (inactive at opioid receptors, so selective for TLR4 activation)[40][50]
Tapentadol (mixed agonist/antagonist)- "Unnatural" isomers such as (+)-morphine activate TLR4 but lack opioid receptor activity,[43] although (+)-morphine also shows activity as a sigma receptor agonist.[56]
Antagonists
- The lipid A analog eritoran acts as a TLR4 antagonist. As of December 2009[update], it was being developed as a drug against severe sepsis.[57] However, in 2013, a news story said the results against sepsis were somewhat disappointing and that it was better used to treat certain cases of severe influenza. Although it does not treat the virus itself, it could be used against the massive immune reaction called cytokine storm which often occurs later in the infection and is a major cause of mortality from severe influenza.[58]
Amitriptyline[51]
Cyclobenzaprine[51]
Ketotifen[51]
Imipramine[51]
Mianserin[51]
Ibudilast[59]
Pinocembrin[60]
Naloxone[50]
Naltrexone[50]- (+)-naltrexone[50]
- LPS-RS[50]
Propentofylline[citation needed]
Tapentadol (mixed agonist/antagonist)
(+)-naloxone ("unnatural" isomer, lacks opioid receptor affinity so selective for TLR4 inhibition)[44]
References
^ abc GRCh38: Ensembl release 89: ENSG00000136869 - Ensembl, May 2017
^ abc GRCm38: Ensembl release 89: ENSMUSG00000039005 - Ensembl, May 2017
^ "Human PubMed Reference:"..mw-parser-output cite.citationfont-style:inherit.mw-parser-output qquotes:"""""""'""'".mw-parser-output code.cs1-codecolor:inherit;background:inherit;border:inherit;padding:inherit.mw-parser-output .cs1-lock-free abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/6/65/Lock-green.svg/9px-Lock-green.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-lock-limited a,.mw-parser-output .cs1-lock-registration abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/d/d6/Lock-gray-alt-2.svg/9px-Lock-gray-alt-2.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-lock-subscription abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/a/aa/Lock-red-alt-2.svg/9px-Lock-red-alt-2.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registrationcolor:#555.mw-parser-output .cs1-subscription span,.mw-parser-output .cs1-registration spanborder-bottom:1px dotted;cursor:help.mw-parser-output .cs1-hidden-errordisplay:none;font-size:100%.mw-parser-output .cs1-visible-errorfont-size:100%.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration,.mw-parser-output .cs1-formatfont-size:95%.mw-parser-output .cs1-kern-left,.mw-parser-output .cs1-kern-wl-leftpadding-left:0.2em.mw-parser-output .cs1-kern-right,.mw-parser-output .cs1-kern-wl-rightpadding-right:0.2em
^ "Mouse PubMed Reference:".
^ ab Vaure C, Liu Y (2014-07-10). "A comparative review of toll-like receptor 4 expression and functionality in different animal species". Frontiers in Immunology. 5: 316. doi:10.3389/fimmu.2014.00316. PMC 4090903. PMID 25071777.
^ Brubaker SW, Bonham KS, Zanoni I, Kagan JC (2015). "Innate immune pattern recognition: a cell biological perspective". Annual Review of Immunology. 33: 257–90. doi:10.1146/annurev-immunol-032414-112240. PMC 5146691. PMID 25581309.
^ "O00206 (TLR4_HUMAN)". Uniprot.
^ abc Lu YC, Yeh WC, Ohashi PS (May 2008). "LPS/TLR4 signal transduction pathway". Cytokine. 42 (2): 145–51. doi:10.1016/j.cyto.2008.01.006. PMID 18304834.
^ "Entrez Gene: TLR4 toll-like receptor 4".
^ ab Korneev KV, Atretkhany KN, Drutskaya MS, Grivennikov SI, Kuprash DV, Nedospasov SA (January 2017). "TLR-signaling and proinflammatory cytokines as drivers of tumorigenesis". Cytokine. 89: 127–135. doi:10.1016/j.cyto.2016.01.021. PMID 26854213.
^ ab O'Neill LA, Golenbock D, Bowie AG (July 2013). "The history of Toll-like receptors - redefining innate immunity". Nature Reviews. Immunology. 13 (6): 453–60. doi:10.1038/nri3446. PMID 23681101.
^ Pålsson-McDermott EM, O'Neill LA (2004). "Signal transduction by the lipopolysaccharide receptor, Toll-like receptor-4". Immunology. 113 (2): 153–62. doi:10.1111/j.1365-2567.2004.01976.x. PMC 1782563. PMID 15379975.
^ Beutler B, Rehli M (2002). "Evolution of the TIR, tolls and TLRs: functional inferences from computational biology". Current Topics in Microbiology and Immunology. 270: 1–21. PMID 12467241.
^ Smirnova I, Poltorak A, Chan EK, McBride C, Beutler B (2000). "Phylogenetic variation and polymorphism at the toll-like receptor 4 locus (TLR4)". Genome Biology. 1 (1): RESEARCH002. doi:10.1186/gb-2000-1-1-research002. PMC 31919. PMID 11104518.
^ Quach H, Wilson D, Laval G, Patin E, Manry J, Guibert J, Barreiro LB, Nerrienet E, Verschoor E, Gessain A, Przeworski M, Quintana-Murci L (December 2013). "Different selective pressures shape the evolution of Toll-like receptors in human and African great ape populations". Human Molecular Genetics. 22 (23): 4829–40. doi:10.1093/hmg/ddt335. PMC 3820138. PMID 23851028.
^ ab Barreiro LB, Ben-Ali M, Quach H, Laval G, Patin E, Pickrell JK, Bouchier C, Tichit M, Neyrolles O, Gicquel B, Kidd JR, Kidd KK, Alcaïs A, Ragimbeau J, Pellegrini S, Abel L, Casanova JL, Quintana-Murci L (July 2009). "Evolutionary dynamics of human Toll-like receptors and their different contributions to host defense". PLoS Genetics. 5 (7): e1000562. doi:10.1371/journal.pgen.1000562. PMC 2702086. PMID 19609346.
^ Plantinga TS, Ioana M, Alonso S, Izagirre N, Hervella M, Joosten LA, van der Meer JW, de la Rúa C, Netea MG (2012). "The evolutionary history of TLR4 polymorphisms in Europe". Journal of Innate Immunity. 4 (2): 168–75. doi:10.1159/000329492. PMID 21968286.
^ Re F, Strominger JL (June 2002). "Monomeric recombinant MD-2 binds toll-like receptor 4 tightly and confers lipopolysaccharide responsiveness". The Journal of Biological Chemistry. 277 (26): 23427–32. doi:10.1074/jbc.M202554200. PMID 11976338.
^ Shimazu R, Akashi S, Ogata H, Nagai Y, Fukudome K, Miyake K, Kimoto M (June 1999). "MD-2, a molecule that confers lipopolysaccharide responsiveness on Toll-like receptor 4". The Journal of Experimental Medicine. 189 (11): 1777–82. doi:10.1084/jem.189.11.1777. PMC 2193086. PMID 10359581.
^ Chuang TH, Ulevitch RJ (May 2004). "Triad3A, an E3 ubiquitin-protein ligase regulating Toll-like receptors". Nature Immunology. 5 (5): 495–502. doi:10.1038/ni1066. PMID 15107846.
^ Doyle SE, O'Connell R, Vaidya SA, Chow EK, Yee K, Cheng G (April 2003). "Toll-like receptor 3 mediates a more potent antiviral response than Toll-like receptor 4". Journal of Immunology. 170 (7): 3565–71. doi:10.4049/jimmunol.170.7.3565. PMID 12646618.
^ Rhee SH, Hwang D (November 2000). "Murine TOLL-like receptor 4 confers lipopolysaccharide responsiveness as determined by activation of NF kappa B and expression of the inducible cyclooxygenase". The Journal of Biological Chemistry. 275 (44): 34035–40. doi:10.1074/jbc.M007386200. PMID 10952994.
^ Fitzgerald KA, Palsson-McDermott EM, Bowie AG, Jefferies CA, Mansell AS, Brady G, Brint E, Dunne A, Gray P, Harte MT, McMurray D, Smith DE, Sims JE, Bird TA, O'Neill LA (September 2001). "Mal (MyD88-adapter-like) is required for Toll-like receptor-4 signal transduction". Nature. 413 (6851): 78–83. doi:10.1038/35092578. PMID 11544529.
^ Zhang G, Ghosh S (March 2002). "Negative regulation of toll-like receptor-mediated signaling by Tollip". The Journal of Biological Chemistry. 277 (9): 7059–65. doi:10.1074/jbc.M109537200. PMID 11751856.
^ Peana M, Zdyb K, Medici S, Pelucelli A, Simula G, Gumienna-Kontecka E, Zoroddu MA (2017). "Ni(II) interaction with a peptide model of the human TLR4 ectodomain". J Trace Elem Med Biol. 44: 151–160. doi:10.1016/j.jtemb.2017.07.006. PMID 28965571.
^ Husebye H, Aune MH, Stenvik J, Samstad E, Skjeldal F, Halaas O, Nilsen NJ, Stenmark H, Latz E, Lien E, Mollnes TE, Bakke O, Espevik T (October 2010). "The Rab11a GTPase controls Toll-like receptor 4-induced activation of interferon regulatory factor-3 on phagosomes". Immunity. 33 (4): 583–96. doi:10.1016/j.immuni.2010.09.010. PMID 20933442.
^ Schröder NW, Schumann RR (March 2005). "Single nucleotide polymorphisms of Toll-like receptors and susceptibility to infectious disease". The Lancet. Infectious Diseases. 5 (3): 156–64. doi:10.1016/S1473-3099(05)01308-3. PMID 15766650.
^ Lorenz E, Mira JP, Frees KL, Schwartz DA (May 2002). "Relevance of mutations in the TLR4 receptor in patients with gram-negative septic shock". Archives of Internal Medicine. 162 (9): 1028–32. doi:10.1001/archinte.162.9.1028. PMID 11996613.
^ Nachtigall I, Tamarkin A, Tafelski S, Weimann A, Rothbart A, Heim S, Wernecke KD, Spies C (February 2014). "Polymorphisms of the toll-like receptor 2 and 4 genes are associated with faster progression and a more severe course of sepsis in critically ill patients". The Journal of International Medical Research. 42 (1): 93–110. doi:10.1177/0300060513504358. PMID 24366499.
^ Pal D, Dasgupta S, Kundu R, Maitra S, Das G, Mukhopadhyay S, Ray S, Majumdar SS, Bhattacharya S (2012). "Fetuin-A acts as an endogenous ligand of TLR4 to promote lipid-induced insulin resistance" (PDF). Nature Medicine. 18 (8): 1279–1285. doi:10.1038/nm.2851. PMID 22842477.
^ ab Mockenhaupt FP, Cramer JP, Hamann L, Stegemann MS, Eckert J, Oh NR, Otchwemah RN, Dietz E, Ehrhardt S, Schröder NW, Bienzle U, Schumann RR (January 2006). "Toll-like receptor (TLR) polymorphisms in African children: Common TLR-4 variants predispose to severe malaria". Proceedings of the National Academy of Sciences of the United States of America. 103 (1): 177–82. doi:10.1073/pnas.0506803102. PMC 1324982. PMID 16371473.
^ Van der Graaf CA, Netea MG, Morré SA, Den Heijer M, Verweij PE, Van der Meer JW, Kullberg BJ (March 2006). "Toll-like receptor 4 Asp299Gly/Thr399Ile polymorphisms are a risk factor for Candida bloodstream infection". European Cytokine Network. 17 (1): 29–34. PMID 16613760.
^ Eyking A, Ey B, Rünzi M, Roig AI, Reis H, Schmid KW, Gerken G, Podolsky DK, Cario E (December 2011). "Toll-like receptor 4 variant D299G induces features of neoplastic progression in Caco-2 intestinal cells and is associated with advanced human colon cancer". Gastroenterology. 141 (6): 2154–65. doi:10.1053/j.gastro.2011.08.043. PMC 3268964. PMID 21920464.
^ Liu J, Yang AR, Kelly T, Puche A, Esoga C, June HL, Elnabawi A, Merchenthaler I, Sieghart W, June HL, Aurelian L (March 2011). "Binge alcohol drinking is associated with GABAA alpha2-regulated Toll-like receptor 4 (TLR4) expression in the central amygdala". Proceedings of the National Academy of Sciences of the United States of America. 108 (11): 4465–70. doi:10.1073/pnas.1019020108. PMC 3060224. PMID 21368176. Lay summary – sciencedaily.com.
^ Blanco AM, Vallés SL, Pascual M, Guerri C (November 2005). "Involvement of TLR4/type I IL-1 receptor signaling in the induction of inflammatory mediators and cell death induced by ethanol in cultured astrocytes". Journal of Immunology. 175 (10): 6893–9. doi:10.4049/jimmunol.175.10.6893. PMID 16272348.
^ Hakim F, Wang Y, Zhang SX, Zheng J, Yolcu ES, Carreras A, Khalyfa A, Shirwan H, Almendros I, Gozal D (March 2014). "Fragmented sleep accelerates tumor growth and progression through recruitment of tumor-associated macrophages and TLR4 signaling". Cancer Research. 74 (5): 1329–37. doi:10.1158/0008-5472.CAN-13-3014. PMC 4247537. PMID 24448240.
^ Shavit Y, Wolf G, Goshen I, Livshits D, Yirmiya R (May 2005). "Interleukin-1 antagonizes morphine analgesia and underlies morphine tolerance". Pain. 115 (1–2): 50–9. doi:10.1016/j.pain.2005.02.003. PMID 15836969.
^ Mohan S, Davis RL, DeSilva U, Stevens CW (October 2010). "Dual regulation of mu opioid receptors in SK-N-SH neuroblastoma cells by morphine and interleukin-1β: evidence for opioid-immune crosstalk". Journal of Neuroimmunology. 227 (1–2): 26–34. doi:10.1016/j.jneuroim.2010.06.007. PMC 2942958. PMID 20615556.
^ Komatsu T, Sakurada S, Katsuyama S, Sanai K, Sakurada T (2009). "Mechanism of allodynia evoked by intrathecal morphine-3-glucuronide in mice". International Review of Neurobiology. International Review of Neurobiology. 85: 207–19. doi:10.1016/S0074-7742(09)85016-2. ISBN 9780123748935. PMID 19607972.
^ ab Lewis SS, Hutchinson MR, Rezvani N, Loram LC, Zhang Y, Maier SF, Rice KC, Watkins LR (January 2010). "Evidence that intrathecal morphine-3-glucuronide may cause pain enhancement via toll-like receptor 4/MD-2 and interleukin-1beta". Neuroscience. 165 (2): 569–83. doi:10.1016/j.neuroscience.2009.10.011. PMC 2795035. PMID 19833175.
^ Shen CH, Tsai RY, Shih MS, Lin SL, Tai YH, Chien CC, Wong CS (February 2011). "Etanercept restores the antinociceptive effect of morphine and suppresses spinal neuroinflammation in morphine-tolerant rats". Anesthesia and Analgesia. 112 (2): 454–9. doi:10.1213/ANE.0b013e3182025b15. PMID 21081778.
^ Hook MA, Washburn SN, Moreno G, Woller SA, Puga D, Lee KH, Grau JW (February 2011). "An IL-1 receptor antagonist blocks a morphine-induced attenuation of locomotor recovery after spinal cord injury". Brain, Behavior, and Immunity. 25 (2): 349–59. doi:10.1016/j.bbi.2010.10.018. PMC 3025088. PMID 20974246.
^ ab Watkins LR, Hutchinson MR, Rice KC, Maier SF (November 2009). "The "toll" of opioid-induced glial activation: improving the clinical efficacy of opioids by targeting glia". Trends in Pharmacological Sciences. 30 (11): 581–91. doi:10.1016/j.tips.2009.08.002. PMC 2783351. PMID 19762094.
^ abc Hutchinson MR, Zhang Y, Brown K, Coats BD, Shridhar M, Sholar PW, Patel SJ, Crysdale NY, Harrison JA, Maier SF, Rice KC, Watkins LR (July 2008). "Non-stereoselective reversal of neuropathic pain by naloxone and naltrexone: involvement of toll-like receptor 4 (TLR4)". The European Journal of Neuroscience. 28 (1): 20–9. doi:10.1111/j.1460-9568.2008.06321.x. PMC 2588470. PMID 18662331.
^ Hutchinson MR, Coats BD, Lewis SS, Zhang Y, Sprunger DB, Rezvani N, Baker EM, Jekich BM, Wieseler JL, Somogyi AA, Martin D, Poole S, Judd CM, Maier SF, Watkins LR (November 2008). "Proinflammatory cytokines oppose opioid-induced acute and chronic analgesia". Brain, Behavior, and Immunity. 22 (8): 1178–89. doi:10.1016/j.bbi.2008.05.004. PMC 2783238. PMID 18599265.
^ Hutchinson MR, Lewis SS, Coats BD, Rezvani N, Zhang Y, Wieseler JL, Somogyi AA, Yin H, Maier SF, Rice KC, Watkins LR (May 2010). "Possible involvement of toll-like receptor 4/myeloid differentiation factor-2 activity of opioid inactive isomers causes spinal proinflammation and related behavioral consequences". Neuroscience. 167 (3): 880–93. doi:10.1016/j.neuroscience.2010.02.011. PMC 2854318. PMID 20178837.
^ Lin SL, Tsai RY, Tai YH, Cherng CH, Wu CT, Yeh CC, Wong CS (February 2010). "Ultra-low dose naloxone upregulates interleukin-10 expression and suppresses neuroinflammation in morphine-tolerant rat spinal cords". Behavioural Brain Research. 207 (1): 30–6. doi:10.1016/j.bbr.2009.09.034. PMID 19799935.
^ "Neuroscience: Making morphine work better". Nature. 484 (7395): 419. 26 April 2012. doi:10.1038/484419a.
^ Drahl C (22 August 2012). "Small Molecules Target Toll-Like Receptors". Chemical & Engineering News.
^ abcdefghijkl Hutchinson MR, Zhang Y, Shridhar M, Evans JH, Buchanan MM, Zhao TX, Slivka PF, Coats BD, Rezvani N, Wieseler J, Hughes TS, Landgraf KE, Chan S, Fong S, Phipps S, Falke JJ, Leinwand LA, Maier SF, Yin H, Rice KC, Watkins LR (January 2010). "Evidence that opioids may have toll-like receptor 4 and MD-2 effects". Brain, Behavior, and Immunity. 24 (1): 83–95. doi:10.1016/j.bbi.2009.08.004. PMC 2788078. PMID 19679181.
^ abcdefg Hutchinson MR, Loram LC, Zhang Y, Shridhar M, Rezvani N, Berkelhammer D, Phipps S, Foster PS, Landgraf K, Falke JJ, Rice KC, Maier SF, Yin H, Watkins LR (June 2010). "Evidence that tricyclic small molecules may possess toll-like receptor and myeloid differentiation protein 2 activity". Neuroscience. 168 (2): 551–63. doi:10.1016/j.neuroscience.2010.03.067. PMC 2872682. PMID 20381591.
^ Pascual M, Baliño P, Alfonso-Loeches S, Aragón CM, Guerri C (June 2011). "Impact of TLR4 on behavioral and cognitive dysfunctions associated with alcohol-induced neuroinflammatory damage". Brain, Behavior, and Immunity. 25 Suppl 1: S80–91. doi:10.1016/j.bbi.2011.02.012. PMID 21352907.
^ Kelley KW, Dantzer R (June 2011). "Alcoholism and inflammation: neuroimmunology of behavioral and mood disorders". Brain, Behavior, and Immunity. 25 Suppl 1: S13–20. doi:10.1016/j.bbi.2010.12.013. PMC 4068736. PMID 21193024.
^ Harris SA, Solomon KR (July 1992). "Percutaneous penetration of 2,4-dichlorophenoxyacetic acid and 2,4-D dimethylamine salt in human volunteers". Journal of Toxicology and Environmental Health. 36 (3): 233–40. doi:10.1080/15287399209531634. PMID 1629934.
^ Monari C, Bistoni F, Casadevall A, Pericolini E, Pietrella D, Kozel TR, Vecchiarelli A (January 2005). "Glucuronoxylomannan, a microbial compound, regulates expression of costimulatory molecules and production of cytokines in macrophages". The Journal of Infectious Diseases. 191 (1): 127–37. doi:10.1086/426511. PMID 15593014.
^ Wu HE, Hong JS, Tseng LF (October 2007). "Stereoselective action of (+)-morphine over (-)-morphine in attenuating the (-)-morphine-produced antinociception via the naloxone-sensitive sigma receptor in the mouse". European Journal of Pharmacology. 571 (2–3): 145–51. doi:10.1016/j.ejphar.2007.06.012. PMC 2080825. PMID 17617400.
^ Tidswell M, Tillis W, Larosa SP, Lynn M, Wittek AE, Kao R, Wheeler J, Gogate J, Opal SM (January 2010). "Phase 2 trial of eritoran tetrasodium (E5564), a toll-like receptor 4 antagonist, in patients with severe sepsis". Critical Care Medicine. 38 (1): 72–83. doi:10.1097/CCM.0b013e3181b07b78. PMID 19661804.
^ "New drug offers novel approach to taming flu virus - Vitals". NBCNews. 1 May 2013.
^ Jia ZJ, Wu FX, Huang QH, Liu JM (April 2012). "[Toll-like receptor 4: the potential therapeutic target for neuropathic pain]". Zhongguo Yi Xue Ke Xue Yuan Xue Bao. Acta Academiae Medicinae Sinicae. 34 (2): 168–73. doi:10.3881/j.issn.1000-503X.2012.02.013. PMID 22776604.
^ Lan X, Han X, Li Q, Li Q, Gao Y, Cheng T, Wan J, Zhu W, Wang J (March 2017). "Pinocembrin protects hemorrhagic brain primarily by inhibiting toll-like receptor 4 and reducing M1 phenotype microglia". Brain, behavior, and immunity. 61: 326–339. doi:10.1016/j.bbi.2016.12.012. PMC 5453178. PMID 28007523.
External links
Toll-Like+Receptor+4 at the US National Library of Medicine Medical Subject Headings (MeSH)