Corticosteroid
| Corticosteroid | |
|---|---|
| Drug class | |
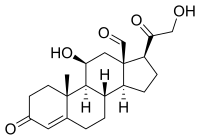
 Cortisol (hydrocortisone), a corticosteroid with both glucocorticoid and mineralocorticoid activity and effects. | |
| Class identifiers | |
| Synonyms | Corticoid |
| Use | Various |
| ATC code | H02 |
| Biological target | Glucocorticoid receptor, Mineralocorticoid receptor |
| Chemical class | Steroids |
| In Wikidata | |
Corticosteroids are a class of steroid hormones that are produced in the adrenal cortex of vertebrates, as well as the synthetic analogues of these hormones. Two main classes of corticosteroids, glucocorticoids and mineralocorticoids, are involved in a wide range of physiological processes, including stress response, immune response, and regulation of inflammation, carbohydrate metabolism, protein catabolism, blood electrolyte levels, and behavior.[1]
Some common naturally occurring steroid hormones are cortisol (C
21H
30O
5), corticosterone (C
21H
30O
4), cortisone (C
21H
28O
5) and aldosterone (C
21H
28O
5). (Note that aldosterone and cortisone share the same chemical formula but the structures are different.) The main corticosteroids produced by the adrenal cortex are cortisol and aldosterone.[2]
.mw-parser-output .toclimit-2 .toclevel-1 ul,.mw-parser-output .toclimit-3 .toclevel-2 ul,.mw-parser-output .toclimit-4 .toclevel-3 ul,.mw-parser-output .toclimit-5 .toclevel-4 ul,.mw-parser-output .toclimit-6 .toclevel-5 ul,.mw-parser-output .toclimit-7 .toclevel-6 uldisplay:none
Contents
1 Classes
2 Medical uses
3 Pharmacogenetics
3.1 Asthma
4 Adverse effects
5 Biosynthesis
6 Classification
6.1 By chemical structure
6.1.1 Group A – Hydrocortisone type
6.1.2 Group B – Acetonides (and related substances)
6.1.3 Group C – Betamethasone type
6.1.4 Group D – Esters
6.1.4.1 Group D1 – Halogenated (less labile)
6.1.4.2 Group D2 – Labile prodrug esters
6.2 By route of administration
6.2.1 Topical steroids
6.2.2 Inhaled steroids
6.2.3 Oral forms
6.2.4 Systemic forms
7 History
7.1 Etymology
8 See also
9 References
Classes

Cortisol

Corticosterone

Cortisone
Aldosterone
Glucocorticoids such as cortisol affect carbohydrate, fat, and protein metabolism, and have anti-inflammatory, immunosuppressive, anti-proliferative, and vasoconstrictive effects.[3] Anti-inflammatory effects are mediated by blocking the action of inflammatory mediators (transrepression) and inducing anti-inflammatory mediators (transactivation).[3] Immunosuppressive effects are mediated by suppressing delayed hypersensitivity reactions by direct action on T-lymphocytes.[3] Anti-proliferative effects are mediated by inhibition of DNA synthesis and epidermal cell turnover.[3] Vasoconstrictive effects are mediated by inhibiting the action of inflammatory mediators such as histidine.[3]
Mineralocorticoids such as aldosterone are primarily involved in the regulation of electrolyte and water balance by modulating ion transport in the epithelial cells of the renal tubules of the kidney.[3]
Medical uses
Synthetic pharmaceutical drugs with corticosteroid-like effects are used in a variety of conditions, ranging from brain tumors to skin diseases. Dexamethasone and its derivatives are almost pure glucocorticoids, while prednisone and its derivatives have some mineralocorticoid action in addition to the glucocorticoid effect. Fludrocortisone (Florinef) is a synthetic mineralocorticoid. Hydrocortisone (cortisol) is typically used for replacement therapy, e.g. for adrenal insufficiency and congenital adrenal hyperplasia.
Medical conditions treated with systemic corticosteroids:[3][4]
Allergy and respirology medicine
Asthma (severe exacerbations)
Chronic obstructive pulmonary disease (COPD)- Allergic rhinitis
- Atopic dermatitis
- Hives
- Angioedema
- Anaphylaxis
- Food allergies
- Drug allergies
- Nasal polyps
- Hypersensitivity pneumonitis
- Sarcoidosis
- Eosinophilic pneumonia
- Some other types of pneumonia (in addition to the traditional antibiotic treatment protocols)
- Interstitial lung disease
Dermatology- Pemphigus vulgaris
- Contact dermatitis
Endocrinology (usually at physiologic doses)- Addison's disease
- Adrenal insufficiency
- Congenital adrenal hyperplasia
Gastroenterology- Ulcerative colitis
- Crohn's disease
- Autoimmune hepatitis
Hematology- Lymphoma
- Leukemia
- Hemolytic anemia
- Idiopathic thrombocytopenic purpura
- Multiple Myeloma
Rheumatology/Immunology- Rheumatoid arthritiseas
- Systemic lupus erythematosus
- Polymyalgia rheumatica
- Polymyositis
- Dermatomyositis
- Polyarteritis
- Vasculitis
Ophthalmology- Uveitis
- Keratoconjunctivitis
- Other conditions
- Multiple sclerosis
- Organ transplantation
- Nephrotic syndrome
Chronic hepatitis (flare ups)- Cerebral edema
- IgG4-related disease
- Prostate cancer
- Tendinosis
- Lichen planus
Topical formulations are also available for the skin, eyes (uveitis), lungs (asthma), nose (rhinitis), and bowels. Corticosteroids are also used supportively to prevent nausea, often in combination with 5-HT3 antagonists (e.g. ondansetron).
Typical undesired effects of glucocorticoids present quite uniformly as drug-induced Cushing's syndrome. Typical mineralocorticoid side-effects are hypertension (abnormally high blood pressure), hypokalemia (low potassium levels in the blood), hypernatremia (high sodium levels in the blood) without causing peripheral edema, metabolic alkalosis and connective tissue weakness.[5] Wound healing or ulcer formation may be inhibited by the immunosuppressive effects.
Clinical and experimental evidence indicates that corticosteroids can cause permanent eye damage by inducing central serous retinopathy (CSR, also known as central serous chorioretinopathy, CSC).[6] A variety of steroid medications, from anti-allergy nasal sprays (Nasonex, Flonase) to topical skin creams, to eye drops (Tobradex), to prednisone have been implicated in the development of CSR.[7][8]
Corticosteroids have been widely used in treating people with traumatic brain injury.[9] A systematic review identified 20 randomised controlled trials and included 12,303 participants, then compared patients who received corticosteroids with patients who received no treatment. The authors recommended people with traumatic head injury should not be routinely treated with corticosteroids.[10]
Pharmacogenetics
Asthma
Patients' response to inhaled corticosteroids has some basis in genetic variations. Two genes of interest are CHRH1 (corticotropin-releasing hormone receptor 1) and TBX21 (transcription factor T-bet). Both genes display some degree of polymorphic variation in humans, which may explain how some patients respond better to inhaled corticosteroid therapy than others.[11][12] However, not all asthma patients respond to corticosteroids and large sub groups of asthma patients are corticosteroid resistant.[13]
Adverse effects

Lower arm of a 47-year-old female showing skin damage caused by topical corticosteroid use.
Use of corticosteroids has numerous side-effects, some of which may be severe:
- Severe amebic colitis: Fulminant amebic colitis is associated with high case fatality and can occur in patients infected with the parasite Entamoeba histolytica after exposure to corticosteroid medications.[14]
- Neuropsychiatric: steroid psychosis,[15] and anxiety,[16]depression. Therapeutic doses may cause a feeling of artificial well-being ("steroid euphoria").[17] The neuropsychiatric effects are partly mediated by sensitization of the body to the actions of adrenaline. Therapeutically, the bulk of corticosteroid dose is given in the morning to mimic the body's diurnal rhythm; if given at night, the feeling of being energized will interfere with sleep. An extensive review is provided by Flores and Gumina.[18]
- Cardiovascular: Corticosteroids can cause sodium retention through a direct action on the kidney, in a manner analogous to the mineralocorticoid aldosterone. This can result in fluid retention and hypertension.
- Metabolic: Corticosteroids cause a movement of body fat to the face and torso, resulting in "moon face", "buffalo hump", and "pot belly" or "beer belly", and cause movement of body fat away from the limbs. This has been termed corticosteroid-induced lipodystrophy. Due to the diversion of amino-acids to glucose, they are considered anti-anabolic, and long term therapy can cause muscle wasting.[19]
- Endocrine: By increasing the production of glucose from amino-acid breakdown and opposing the action of insulin, corticosteroids can cause hyperglycemia,[20]insulin resistance and diabetes mellitus.[21]
- Skeletal: Steroid-induced osteoporosis may be a side-effect of long-term corticosteroid use. Use of inhaled corticosteroids among children with asthma may result in decreased height.[22]
- Gastro-intestinal: While cases of colitis have been reported, corticosteroids are often prescribed when the colitis, although due to suppression of the immune response to pathogens, should be considered only after ruling out infection or microbe/fungal overgrowth in the gastrointestinal tract. While the evidence for corticosteroids causing peptic ulceration is relatively poor except for high doses taken for over a month,[23] the majority of doctors as of 2010[update] still believe this is the case, and would consider protective prophylactic measures.[24]
- Eyes: chronic use may predispose to cataract and retinopathy.
- Vulnerability to infection: By suppressing immune reactions (which is one of the main reasons for their use in allergies), steroids may cause infections to flare up, notably candidiasis.[25]
- Pregnancy: Corticosteroids have a low but significant teratogenic effect, causing a few birth defects per 1,000 pregnant women treated. Corticosteroids are therefore contraindicated in pregnancy.[26]
- Habituation: Topical steroid addiction (TSA) has been reported in long-term users of topical steroids (users who applied topical steroids to their skin over a period of weeks, months, or years).[27][28] TSA is characterised by uncontrollable, spreading dermatitis and worsening skin inflammation which requires a stronger topical steroid to get the same result as the first prescription. When topical steroid medication is lost, the skin experiences redness, burning, itching, hot skin, swelling, and/or oozing for a length of time. This is also called 'red skin syndrome' or 'topical steroid withdrawal'(TSW). After the withdrawal period is over the atopic dermatitis can cease or is less severe than it was before.[29]
- In children the short term use of steroids by mouth increases the risk of vomiting, behavioral changes, and sleeping problems.[30]
Biosynthesis

Steroidogenesis, including corticosteroid biosynthesis.
The corticosteroids are synthesized from cholesterol within the adrenal cortex.[1] Most steroidogenic reactions are catalysed by enzymes of the cytochrome P450 family. They are located within the mitochondria and require adrenodoxin as a cofactor (except 21-hydroxylase and 17α-hydroxylase).
Aldosterone and corticosterone share the first part of their biosynthetic pathway. The last part is mediated either by the aldosterone synthase (for aldosterone) or by the 11β-hydroxylase (for corticosterone). These enzymes are nearly identical (they share 11β-hydroxylation and 18-hydroxylation functions), but aldosterone synthase is also able to perform an 18-oxidation. Moreover, aldosterone synthase is found within the zona glomerulosa at the outer edge of the adrenal cortex; 11β-hydroxylase is found in the zona fasciculata and zona glomerulosa.
Classification
By chemical structure
In general, corticosteroids are grouped into four classes, based on chemical structure. Allergic reactions to one member of a class typically indicate an intolerance of all members of the class. This is known as the "Coopman classification".[31][32]
The highlighted steroids are often used in the screening of allergies to topical steroids.[33]
Group A – Hydrocortisone type
Amcinonide, budesonide, desonide, fluocinolone acetonide, fluocinonide, halcinonide, and triamcinolone acetonide.
Group C – Betamethasone type
Beclometasone, betamethasone, dexamethasone, fluocortolone, halometasone, and mometasone.
Group D – Esters
Group D1 – Halogenated (less labile)
Alclometasone dipropionate, betamethasone dipropionate, betamethasone valerate, clobetasol propionate, clobetasone butyrate, fluprednidene acetate, and mometasone furoate.
Group D2 – Labile prodrug esters
Ciclesonide, cortisone acetate, hydrocortisone aceponate, hydrocortisone acetate, hydrocortisone buteprate, hydrocortisone butyrate, hydrocortisone valerate, prednicarbate, and tixocortol pivalate.
By route of administration
Topical steroids
For use topically on the skin, eye, and mucous membranes.
Topical corticosteroids are divided in potency classes I to IV in most countries (A to D in Japan). Seven categories are used in the United States to determine the level of potency of any given topical corticosteroid.
Inhaled steroids
For nasal mucosa, sinuses, bronchii, and lungs.[34]
This group includes:
Flunisolide[35]
Fluticasone furoate[35]
Fluticasone propionate[35]
Triamcinolone acetonide[35]
Beclomethasone dipropionate[35]
Budesonide[35]
There also exist certain combination preparations such as Advair Diskus in the United States, containing fluticasone propionate and salmeterol (a long-acting bronchodilator), and Symbicort, containing budesonide and formoterol fumarate dihydrate (another long-acting bronchodilator).[35] They are both approved for use in children over 12 years old.
Oral forms
Such as prednisone, prednisolone, methylprednisolone, or dexamethasone.[36]
Systemic forms
Available in injectables for intravenous and parenteral routes.[36]
History
| Corticosteroid | Introduced |
|---|---|
| Cortisone | 1948 |
| Hydrocortisone | 1951 |
| Fludrocortisone acetate | 1954[40] |
| Prednisolone | 1955 |
| Prednisone | 1955[41] |
| Methylprednisolone | 1956 |
| Triamcinolone | 1956 |
| Dexamethasone | 1958 |
| Betamethasone | 1958 |
| Triamcinolone acetonide | 1958 |
| Fluorometholone | 1959 |
Tadeusz Reichstein, Edward Calvin Kendall. and Philip Showalter Hench were awarded the Nobel Prize for Physiology and Medicine in 1950 for their work on hormones of the adrenal cortex, which culminated in the isolation of cortisone.[42]
Initially hailed as a miracle cure and liberally prescribed during the 1950s, steroid treatment brought about adverse events of such a magnitude that the next major category of anti-inflammatory drugs, the nonsteroidal anti-inflammatory drugs (NSAIDs), was so named in order to demarcate from the opprobrium.[43] Corticosteroids were voted Allergen of the Year in 2005 by the American Contact Dermatitis Society.[44]
Lewis Sarett of Merck & Co. was the first to synthesize cortisone, using a 36-step process that started with deoxycholic acid, which was extracted from ox bile.[45] The low efficiency of converting deoxycholic acid into cortisone led to a cost of US $200 per gram. Russell Marker, at Syntex, discovered a much cheaper and more convenient starting material, diosgenin from wild Mexican yams. His conversion of diosgenin into progesterone by a four-step process now known as Marker degradation was an important step in mass production of all steroidal hormones, including cortisone and chemicals used in hormonal contraception.[46]
In 1952, D.H. Peterson and H.C. Murray of Upjohn developed a process that used Rhizopus mold to oxidize progesterone into a compound that was readily converted to cortisone.[47] The ability to cheaply synthesize large quantities of cortisone from the diosgenin in yams resulted in a rapid drop in price to US $6 per gram, falling to $0.46 per gram by 1980. Percy Julian's research also aided progress in the field.[48] The exact nature of cortisone's anti-inflammatory action remained a mystery for years after, however, until the leukocyte adhesion cascade and the role of phospholipase A2 in the production of prostaglandins and leukotrienes was fully understood in the early 1980s.
Etymology
The cortico- part of the name refers to the adrenal cortex, which makes these steroid hormones. Thus a corticosteroid is a "cortex steroid".
See also
 Corticosteroids portal
Corticosteroids portal- List of corticosteroids
- List of corticosteroid cyclic ketals
- List of corticosteroid esters
- List of steroid abbreviations
References
^ ab Nussey, S.; Whitehead, S. (2001). Endocrinology: An Integrated Approach. Oxford: BIOS Scientific Publishers..mw-parser-output cite.citationfont-style:inherit.mw-parser-output .citation qquotes:"""""""'""'".mw-parser-output .citation .cs1-lock-free abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/6/65/Lock-green.svg/9px-Lock-green.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .citation .cs1-lock-limited a,.mw-parser-output .citation .cs1-lock-registration abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/d/d6/Lock-gray-alt-2.svg/9px-Lock-gray-alt-2.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .citation .cs1-lock-subscription abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/a/aa/Lock-red-alt-2.svg/9px-Lock-red-alt-2.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registrationcolor:#555.mw-parser-output .cs1-subscription span,.mw-parser-output .cs1-registration spanborder-bottom:1px dotted;cursor:help.mw-parser-output .cs1-ws-icon abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/4/4c/Wikisource-logo.svg/12px-Wikisource-logo.svg.png")no-repeat;background-position:right .1em center.mw-parser-output code.cs1-codecolor:inherit;background:inherit;border:inherit;padding:inherit.mw-parser-output .cs1-hidden-errordisplay:none;font-size:100%.mw-parser-output .cs1-visible-errorfont-size:100%.mw-parser-output .cs1-maintdisplay:none;color:#33aa33;margin-left:0.3em.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration,.mw-parser-output .cs1-formatfont-size:95%.mw-parser-output .cs1-kern-left,.mw-parser-output .cs1-kern-wl-leftpadding-left:0.2em.mw-parser-output .cs1-kern-right,.mw-parser-output .cs1-kern-wl-rightpadding-right:0.2em
^ Nussey, Stephen; Whitehead, Saffron (2001-01-01). The adrenal gland. BIOS Scientific Publishers.
^ abcdefg Liu, Dora; Ahmet, Alexandra; Ward, Leanne; Krishnamoorthy, Preetha; Mandelcorn, Efrem D; Leigh, Richard; Brown, Jacques P; Cohen, Albert; Kim, Harold (2013-08-15). "A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy". Allergy, Asthma, and Clinical Immunology. 9 (1): 30. doi:10.1186/1710-1492-9-30. ISSN 1710-1484. PMC 3765115. PMID 23947590.
^ Mohamadi, Amin; Chan, Jimmy J.; Claessen, Femke M. A. P.; Ring, David; Chen, Neal C. (2017-01-01). "Corticosteroid Injections Give Small and Transient Pain Relief in Rotator Cuff Tendinosis: A Meta-analysis". Clinical Orthopaedics and Related Research. 475 (1): 232–243. doi:10.1007/s11999-016-5002-1. ISSN 0009-921X. PMC 5174041. PMID 27469590.
^ Werner R (2005). A massage therapist's guide to Pathology (3rd ed.). Pennsylvania: Lippincott Williams & Wilkins.
^ Abouammoh, Marwan A. (2015). "Advances in the treatment of central serous chorioretinopathy". Saudi Journal of Ophthalmology. 29 (4): 278–286. doi:10.1016/j.sjopt.2015.01.007. ISSN 1319-4534. PMC 4625218. PMID 26586979.
^ Carvalho-Recchia, CA; Yannuzzi, LA; Negrão, S; Spaide, RF; Freund, KB; Rodriguez-Coleman, H; Lenharo, M; Iida, T (2002). "Corticosteroids and central serous chorioretinopathy". Ophthalmology. 109 (10): 1834–7. doi:10.1016/S0161-6420(02)01117-X. PMID 12359603.
^ "The New York Times :: A Breathing Technique Offers Help for People With Asthma". buteykola.com. Retrieved 2012-11-30.
^ Alderson P, Roberts I. "Plain Language Summary". Corticosteroids for acute traumatic brain injury. The Cochrane Collaboration. p. 2.
^ Alderson, P.; Roberts, I. (2005). Alderson, Phil, ed. "Corticosteroids for acute traumatic brain injury". Cochrane Database Syst Rev (1): CD000196. doi:10.1002/14651858.CD000196.pub2. PMID 15674869.
^ Tantisira KG, Lake S, Silverman ES, Palmer LJ, Lazarus R, Silverman EK, Liggett SB, Gelfand EW, Rosenwasser LJ, Richter B, Israel E, Wechsler M, Gabriel S, Altshuler D, Lander E, Drazen J, Weiss ST (2004). "Corticosteroid pharmacogenetics: association of sequence variants in CRHR1 with improved lung function in asthmatics treated with inhaled corticosteroids". Human Molecular Genetics. 13 (13): 1353–9. doi:10.1093/hmg/ddh149. PMID 15128701.
^ Tantisira KG, Hwang ES, Raby BA, Silverman ES, Lake SL, Richter BG, Peng SL, Drazen JM, Glimcher LH, Weiss ST (Dec 2004). "TBX21: A functional variant predicts improvement in asthma with the use of inhaled corticosteroids". PNAS. 101 (52): 18099–18104. Bibcode:2004PNAS..10118099T. doi:10.1073/pnas.0408532102. PMC 539815. PMID 15604153.
^ Peters, Michael C.; Kerr, Sheena; Dunican, Eleanor M.; Woodruff, Prescott G.; Fajt, Merritt L.; Levy, Bruce D.; Israel, Elliot; Phillips, Brenda R.; Mauger, David T.; Comhair, Suzy A.; Erzurum, Serpil C.; Johansson, Mats W.; Jarjour, Nizar N.; Coverstone, Andrea M.; Castro, Mario; Hastie, Annette T.; Bleecker, Eugene R.; Wenzel, Sally E.; Fahy, John V. (March 2018). "Refractory airway type 2 inflammation in a large subgroup of asthmatic patients treated with inhaled corticosteroids". Journal of Allergy and Clinical Immunology. 143 (1): 104–113.e14. doi:10.1016/j.jaci.2017.12.1009. PMC 6128784. PMID 29524537.
^ Shirley, Debbie-Ann; Moonah, Shannon; Meza, Isaura (28 July 2016). "Fulminant Amebic Colitis after Corticosteroid Therapy: A Systematic Review". PLOS Neglected Tropical Diseases. 10 (7): e0004879. doi:10.1371/journal.pntd.0004879. PMC 4965027. PMID 27467600.
^ Hall, Richard. "Psychiatric Adverse Drug Reactions: Steroid Psychosis". Director of Research Monarch Health Corporation Marblehead, Massachusetts.
^ Korte SM (2001). "Corticosteroids in relation to fear, anxiety and psychopathology". Neurosci Biobehav Rev. 25 (2): 117–42. doi:10.1016/S0149-7634(01)00002-1. PMID 11323078.
^ Swinburn CR, Wakefield JM, Newman SP, Jones PW (December 1988). "Evidence of prednisolone induced mood change ('steroid euphoria') in patients with chronic obstructive airways disease". Br J Clin Pharmacol. 26 (6): 709–713. doi:10.1111/j.1365-2125.1988.tb05309.x. PMC 1386585. PMID 3242575.
^ Benjamin H. Flores and Heather Kenna Gumina. The Neuropsychiatric Sequelae of Steroid Treatment. URL:http://www.dianafoundation.com/articles/df_04_article_01_steroids_pg01.html
^ Hasselgren PO, Alamdari N, Aversa Z, Gonnella P, Smith IJ, Tizio S (July 2010). "CORTICOSTEROIDS AND MUSCLE WASTING ROLE OF TRANSCRIPTION FACTORS, NUCLEAR COFACTORS, AND HYPERACETYLATION". Curr Opin Clin Nutr Metab Care. 13 (4): 423–428. doi:10.1097/MCO.0b013e32833a5107. PMC 2911625. PMID 20473154.
^ Donihi AC, Raval D, Saul M, Korytkowski MT, DeVita MA (2006). "Prevalence and predictors of corticosteroid-related hyperglycemia in hospitalized patients". Endocr Pract. 12 (4): 358–62. doi:10.4158/ep.12.4.358. PMID 16901792.
^ Blackburn D, Hux J, Mamdani M (2007). "Quantification of the risk of corticosteroid-induced diabetes mellitus among the elderly". Journal of General Internal Medicine. 17 (9): 717–720. doi:10.1046/j.1525-1497.2002.10649.x. PMC 1495107. PMID 12220369.
^ Zhang, L; Prietsch, SO; Ducharme, FM (Jul 17, 2014). "Inhaled corticosteroids in children with persistent asthma: effects on growth". The Cochrane Database of Systematic Reviews. 7 (7): CD009471. doi:10.1002/14651858.CD009471.pub2. PMID 25030198.
^ Pecora PG, Kaplan B (1996). "Corticosteroids and ulcers: is there an association?". Ann Pharmacother. 30 (7–8): 870–2. doi:10.1177/106002809603000729. PMID 8826575.
^ Martínek J, Hlavova K, Zavada F, et al. (June 2010). ""A surviving myth" —corticosteroids are still considered ulcerogenic by a majority of physicians". Scand J Gastroenterol. 45 (10): 1156–61. doi:10.3109/00365521.2010.497935. PMID 20569095.
^ Fukushima, C.; Matsuse, H.; Tomari, S.; Obase, Y.; Miyazaki, Y.; Shimoda, T.; Kohno, S. (2003). "Oral candidiasis associated with inhaled corticosteroid use: Comparison of fluticasone and beclomethasone". Annals of Allergy, Asthma & Immunology. 90 (6): 646–651. doi:10.1016/S1081-1206(10)61870-4. PMID 12839324.
^ Shepard, TH.; Brent, RL.; Friedman, JM.; Jones, KL.; Miller, RK.; Moore, CA.; Polifka, JE. (April 2002). "Update on new developments in the study of human teratogens". Teratology. 65 (4): 153–61. doi:10.1002/tera.10032. PMID 11948561.
^ Nnoruka, Edith; Daramola, Olaniyi; Ike, Samuel (2007). "Misuse and abuse of topical steroids: implications". Expert Review of Dermatology. 2 (1): 31–40. doi:10.1586/17469872.2.1.31. Retrieved 2014-12-18.
^ Sanjay, Rathi; D'Souza, Paschal (2012). "Rational and ethical use of topical corticosteroids based on safety and efficacy". Indian Journal of Dermatology. 57 (4): 251–259. doi:10.4103/0019-5154.97655. PMC 3401837. PMID 22837556.
^ Fukaya, M; Sato, K; Sato, M; Kimata, H; Fujisawa, S; Dozono, H; Yoshizawa, J; Minaguchi, S (2014). "Topical steroid addiction in atopic dermatitis". Drug, Healthcare and Patient Safety. 6: 131–8. doi:10.2147/dhps.s69201. PMC 4207549. PMID 25378953.
^ Aljebab, F; Choonara, I; Conroy, S (April 2016). "Systematic review of the toxicity of short-course oral corticosteroids in children". Archives of Disease in Childhood. 101 (4): 365–70. doi:10.1136/archdischild-2015-309522. PMC 4819633. PMID 26768830.
^ Rietschel, Robert L. (2007). Fisher's Contact Dermatitis, 6/e. Hamilton, Ont: BC Decker Inc. p. 256. ISBN 978-1-55009-378-0.
^ Coopman S, Degreef H, Dooms-Goossens A (July 1989). "Identification of cross-reaction patterns in allergic contact dermatitis from topical corticosteroids". Br. J. Dermatol. 121 (1): 27–34. doi:10.1111/j.1365-2133.1989.tb01396.x. PMID 2757954.
^ Wolverton, SE (2001). Comprehensive Dermatologic Drug Therapy. WB Saunders. p. 562.
^ "Asthma Steroids: Inhaled Steroids, Side Effects, Benefits, and More". Webmd.com. Retrieved 2012-11-30.
^ abcdefg Mayo Clinic Staff (September 2015). "Asthma Medications: Know your options". MayoClinic.org. Retrieved 2018-02-27.
^ ab "Systemic steroids (corticosteroids). DermNet NZ". . DermNet NZ. 2012-05-19. Retrieved 2012-11-30.
^ Khan MO, Park KK, Lee HJ (2005). "Antedrugs: an approach to safer drugs". Curr. Med. Chem. 12 (19): 2227–39. doi:10.2174/0929867054864840. PMID 16178782.
^ Calvert DN (1962). "Anti-inflammatory steroids". Wis. Med. J. 61: 403–4. PMID 13875857.
^ Alberto Conde-Taboada (2012). Dermatological Treatments. Bentham Science Publishers. pp. 35–36. ISBN 978-1-60805-234-9.
^ William Andrew Publishing (22 October 2013). Pharmaceutical Manufacturing Encyclopedia, 3rd Edition. Elsevier. pp. 1642–1643. ISBN 978-0-8155-1856-3.
^ Kyu-Won Kim; Jae Kyung Roh; Hee-Jun Wee; Chan Kim (14 November 2016). Cancer Drug Discovery: Science and History. Springer. pp. 169–. ISBN 978-94-024-0844-7.
^ http://nobelprize.org/nobel_prizes/medicine/laureates/1950/kendall-lecture.pdf
^ Buer JK (Oct 2014). "Origins and impact of the term 'NSAID'" (PDF). Inflammopharmacology. 22 (5): 263–7. doi:10.1007/s10787-014-0211-2. hdl:10852/45403. PMID 25064056.
^ "Contact Allergen of the Year: Corticosteroids: Introduction". Medscape.com. 2005-06-13. Retrieved 2012-11-30.
^ Sarett, Lewis H. (1947). "Process of Treating Pregnene Compounds", U. S. Patent 2,462,133
^ Marker, Russell E.; Wagner, R. B.; Ulshafer, Paul R.; Wittbecker, Emerson L.; Goldsmith, Dale P. J.; Ruof, Clarence H. (1947). "Steroidal Sapogenins". J. Am. Chem. Soc. 69 (9): 2167–2230. doi:10.1021/ja01201a032. PMID 20262743.
^ Peterson DH, Murray HC (1952). "Microbiological Oxygenation of Steroids at Carbon 11". J. Am. Chem. Soc. 74 (7): 1871–2. doi:10.1021/ja01127a531.
^ Julian, Percy L., Cole, John Wayne, Meyer, Edwin W., and Karpel, William J. (1956) "Preparation of Cortisone". U. S. Patent 2,752,339
